Keratoconus contact lens fitting
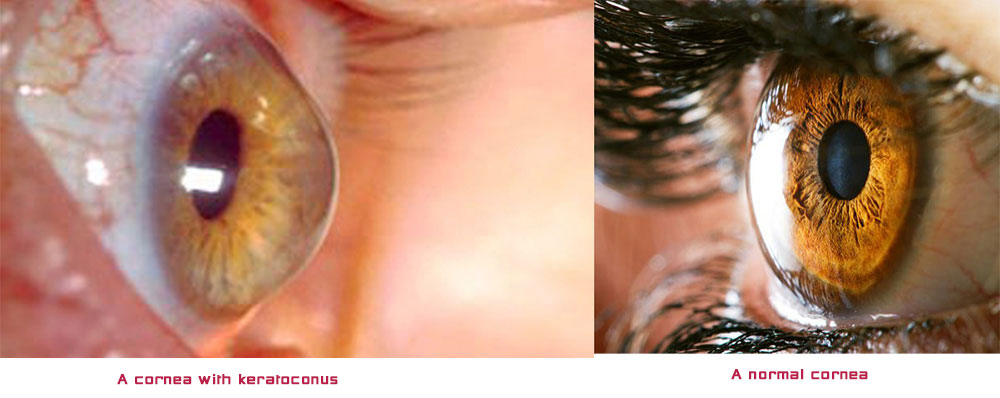
Keratoconus is a non-inflammatory, usually slow progressive eye disorder in which the normal spherical shaped cornea (the outer most transparent tissue/window of the eye) thins and progressively protrudes into a cone-like shape. This changed shape, is irregular and since the cornea is responsible for refracting most of the light entering the eye, an irregular cornea usually suffers from high refractive errors and especially high irregular astigmatism and therefore causes blurred and distorted vision.
Keratoconus is a non-inflammatory, usually slow progressive eye disorder in which the normal spherical shaped cornea (the outer most transparent tissue/window of the eye) thins and progressively protrudes into a cone-like shape. This changed shape, is irregular and since the cornea is responsible for refracting most of the light entering the eye, an irregular cornea usually suffers from high refractive errors and especially high irregular astigmatism and therefore causes blurred and distorted vision. Keratoconus can affect one or both eyes, it tends to progress less and in a slower rate if diagnosed after the age of 25. However it can occur during puberty and early management is very important. Keratoconus is the most frequently seen corneal ectasia with a prevalence of 1 in 1000. This number is thought to be much higher around our region, the region of the eastern Mediterranean. The cause of all corneal ectasias is not really known, even though there is most certainly a genetic predisposition for their inheritance.
In moderate or progressed cases of keratoconus, this distorted vision can no longer be corrected with glasses but only with specialized contact lens fitting. Corneal grafting or corneal transplant is a major operation for the eye and involves corneal tissue from a donor being transplanted on to the central part of the cornea of the patient. Experienced surgeons agree that corneal transplantation must be offered as the final solution to patients and only if everything else has failed to give adequate and comfortable vision. This is because a corneal graft will not make all problems disappear and will not exactly take you back into the days when you had no keratoconus. Even though corneal grafts are without a doubt in many cases sight savers, the management of keratoconus with experienced specialized contact lens fitting should be the first choice for as long as possible. There are tremendous developments in the contact lens fitting of patients who suffer from keratoconus and a patient must be seen by an experience optometrist who has worked in the field of fitting such cases before ending up on the operating table for a corneal graft. Moreover, according to a study carried out at London’s Moorfiels Eye Hospital, about 30 to 50% of grafted patients still require specialized contact lens fitting after surgery (please see separate page dedicated to post graft contact lens fitting).
After careful examination and depending on your cone shape (nipple cone, oval cone or globus cone) and the stage of your keratoconus (mild, moderate or severe), your optometrist will decide which one of the following Keratoconus specialized contact lens fitting offers is best for you:
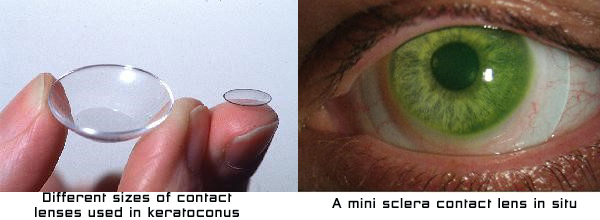
- Small to medium diameter keratoconic contact lens designs offered in gas permeable materials
- Soft lens materials manufactured especially for keratoconus
- Hybrid keratoconic lens designs involving a gas permeable center surrounded with a soft skirt around its perimeter
- Piggy back combination lenses which involve a rigid gas permeable lens resting on a soft lens which can be a daily soft lens or a monthly soft lens with no power in it, for greater comfort
- Larger diameter gas permeable lenses especially designed for keratoconus
- Mini scleral lenses offered again in gas permeable materials (these lenses are larger in diameter than option 1 and 5) and might go up to 15mm in diameter), their periphery resting on the sclera which is the white part of your eye
Please do NOT rub your eyes under any circumstances if you have been diagnosed with keratoconus. Whether you use contact lenses or not, whether your keratoconus is mild, moderate or progressed don’t do it. It is generally agreed by ophthalmologists and optometrists that rubbing your corneas can actually worsen your condition and cause further scarring to your thinned corneas.
If you have keratoconus, please DON’T RUB!!
- Please do NOT rub your eyes under any circumstances if you have been diagnosed with keratoconus. Whether you use contact lenses or not, whether your keratoconus is mild, moderate or progressed don’t do it. It is generally agreed by ophthalmologists and optometrists that rubbing your corneas can actually worsen your condition and cause further scarring to your thinned corneas. Most people who have keratoconus, also suffer by eye allergies and the reason for eye itching should be well established initially by your ophthalmologist. The worse time of the day according to patients who have keratoconus, is clearly just after they remove their lenses. So try to rub around the eyes if you must, but DO NOT rub your corneas. Have a cold gel pack or compress by your site and use it over your closed eyes while you relax, every time you remove your contact lenses.
- If you are a young active person and you have just been diagnosed with keratoconus, don’t be upset and try not to worry too much. There is a lot that can be done for you. Just think that having keratoconus, probably means that you will be wearing a special kind of contact lenses compared to some of your friends who do wear contact lenses anyway
- If you have keratoconus and you are in contact lenses already, do keep your contact lens follow up appointments even if your vision in your lenses is good and even if you are comfortable in your lenses for most of the day. It is important for your optometrist to check the health of your cornea, the condition and fit of your contact lenses at least once every six months unless advised otherwise
- Take good care of your contact lenses, cleaning and caring for them is as important as taking caring of your eyes. Clean them in the evening before you store them and never use tap water to rinse the cleaner away (only sterilized saline solution). Only use the correct solutions for the type of contact lenses that you use and be particularly cautious if your contact lenses are made of gas permeable materials; only use a cleaner and a conditioning solution made for gas permeable materials
Other corneal ectasias:
Keratoglobus
Keratoglobus is a rare non-inflammatoty corneal thinning disorter characterized by generalized thinning and globular protrusion of the cornea. Keratoglobus can be congenital and if present from birth is always bilateral. Congenital keratoglobus has been connected with connective tissue systemic disorters such as Marfan’s syndrome. The acquired forms of keratoglobus have been described in association with other eye pathology such as chronic marginal blepharitis and dysthyroid eye disease. The exact aetiology and genetic inheritance of keratoglobus are still not completely understood. The clinical presentation of patients with keratoglobus is characterized by progressive corneal fragility due to extreme thinning.
Pellucid Marginal Degeneration
Pellucid Marginal Degeneration (PMD) is the second most prevalent condition after Keratoconus, that causes slow clear bilateral thinning of the cornea leading to deterioration of the vision as the corneal shape changes. The thinning of the cornea, involves the inferior and peripheral region of the cornea whereas the thickness of the central cornea remains normal. The inferior peripheral thinning of the cornea is typically seen between the 4 and 8 o’clock positions.




